Sacroiliac (SI) joint pain is a challenging condition affecting 15% to 25% of patients with axial low back pain, for which there is no standard long-term treatment. Recent studies have demonstrated that historical and physical examination findings and radiological imaging are insufficient to diagnose SI joint pain. The most commonly used method to diagnose the SI joint as a pain generator is with smallvolume local anesthetic blocks. In the article, I will try to explain the diagnostic methods and available treatments in detail.
Structure and Function of the SI joint
The sacroiliac joint is the largest axial joint in the body, with an average surface area of 17.5 cm2 [1]. There is wide variability in the adult SI joint [2, 3]. The SI joint is most often characterised as a large, auricularshaped, diarthrodial synovial joint. It has no joint capsule at the posterior and is covered by an extensive ligamentous structure, functioning as a connecting band between the sacrum and ilia. The ligaments are serving a static stabiliser to the joint. (Fig. 1) In addition, the SI joint is also supported by a network of muscles (gluteus maximus, piriformis and biceps femoris) that help to stabilise the pelvic bones.
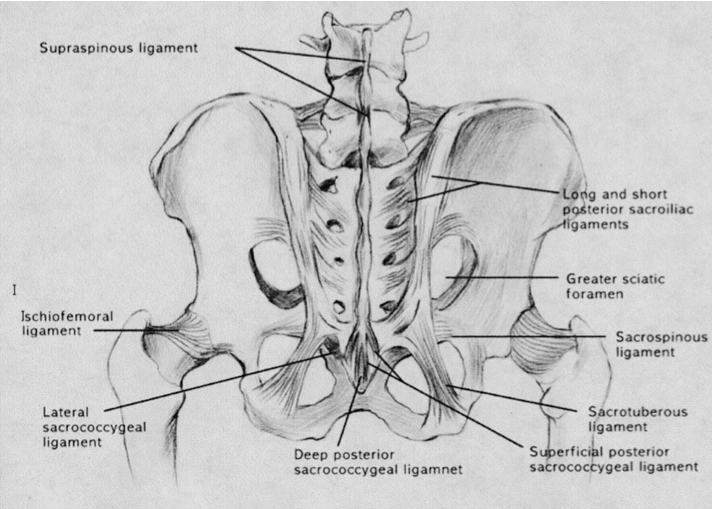
Fig 1. Posterior ligamentous structures stabilizing sacroiliac joint.
Normal Aging of SI joint
Age-related changes in the SI joint begin in puberty and continue throughout life. Degenerative x-ray changes are usually found by the third and fourth decades. In the sixth decade, motion at the joint may become markedly restricted as the capsule becomes increasingly rigid.
Nerve supply to SI joint
The innervation of the SI joint remains a subject of much debate. Some authors have suggested that the anterior SI joint is devoid of nervous tissue [4, 5]. However, it is commonly believed that the lateral branches of the L5-S3 dorsal rami are responsible for the major nerve supply to the posterior SI joint [1].
Prevalence
Bernard and Kirkaldy-Willis, who performed the largest prevalence study, found that 22.5% of patients presenting with low back pain were suffering from SI joint pain [6]. By using criteria based on International Spinal Injection Society guidelines [7], the prevalence of SI joint pain in carefully screened LBP patients appears to be 15%–25% [8].