Summary
Cervical disc hernia with spinal cord or nerve root compression is a common disease. It is common in younger population including those without special risk factors. Surgical treatment has good outcomes if conservative treatment fail. The surgical risk is not high. There are newer technology to overcome the problem of the past in reducing the surgical risk and speeding recovery.
Overview
First line treatment for most cervical disc problems is pain control and physical therapies. Second line treatment includes injections and radiofrequency neurotomy. If this approach fails, or if there is significant neurological deficit, surgical treatment is appropriate.
Anterior Cervical Discectomy and Fusion (ACDF) or Artifical Disc Replacement (ADR) are common surgical procedures performed to treat the herniated or degenerative disc in the cervical (neck) spine. The surgeon approaches the spine from the front, the vertebrae above and below the disc space are fused together or replaced with a new "joint". Patients typically stay overnight and the recovery time takes 3-4 weeks.


Discectomy means “removing the disc”. A discectomy can be performed anywhere along the spine from the neck (cervical) to the lower back (lumbar). In the cervical region, the surgeon reaches the damaged disc from the front (anterior) of the spine – through the throat area. By moving aside the neck muscles, trachea, and oesophagus, the disc and the bony vertebrae are accessed. In the neck, anterior approach is a safe and convenient approach than the posterior because the disc can be reached without disturbing the spinal cord, spinal nerves and the strong neck muscles at the back of the neck [1]. Depending on your situation, your doctor may suggest you to have one (single) level or more than one (multiple) level discectomy and fusion.
After the disc is removed, the space between the bony vertebrae is empty. To prevent the vertebrae from collapsing and rubbing together, the open space is usually filled by a bone graft or substitute. The bone graft serves a bridge between the two vertebrae to create a spinal fusion. The bone graft and vertebrae are often immobilised and held together with metal plates and screws. Following surgery the body begins its natural healing process and new hone cells are formed around the graft. After 3 to 6 months, the bone graft should join the vertebrae above and below to form one solid piece of bone [2]. With instrumentation and fusion working together, the bone may actually grow around the plates and screws – similar to reinforced concrete [3].
Bone grafts come from many sources. Each type has advantages and disadvantages.
- Autograft bone comes from you. The surgeon takes your own bone cells from the pelvis (iliac crest) and transplants to the fusion site. The graft has a higher rate of fusion because it has bone-growing cells and proteins. The drawback is the pain in your hip will cause more pain than the neck wound. Extra-surgery time is required for harvesting the bone from the hip at the same time as the spine surgery. Complications such as donor site pain, infection, fracture of the pelvic bone happen sometimes. Therefore, autograft is not the in favour in most situations.
- Allograft bone comes from a donor (cadaver). The allograft is usually provided by a local bone bank which collects the bone from people who have agreed to donate their tissue after they die. Although screening of all known infectious disease has been performed, contamination of the bone graft causing deep seated infection of the spine is also reported occasionally. Disease transmission such as HIV, Hepatitis virus or even ‘mad cow disease’ is always a potential risk. However, allograft is an unlimited source of bone graft. If your own bone is osteoporotic (not good for structural support in the spine), allograft might be a better choice.
- Bone substitute comes from fully synthetic substance - plastic, ceramic, or bioresorbable compounds. It has no risk of disease transmission from one person to the others. The supply is also theoretically unlimited. The only limitation is the bone healing is slightly inferior to the autograft. The cost is relatively higher than the allograft and autograft.
After fusion, you may notice some range of motion loss, but this varies according to neck mobility before surgery and the number of levels fused. If only one level is fused, you may have similar or even better range of motion than before surgery. If more than two levels are fused, you may notice limits in turning your head and looking up and down. For each fusion level, the theoretically motion loss will be around 12-14 degrees [4]. New motion-preservation artificial disc replacements (ADR) have emerged as an alternative to fusion. Similar to knee replacement, the artificial disc is inserted into the damaged joint space (intervertebral disc space) and preserved the motion, whereas fusion eliminates motion. Outcomes for artificial disc replacement compared to fusion (gold standard surgery) are similar, but long term results of motion preservation and adjacent level disease are still under observation [5].


ACDF may be helpful in treating the following conditions:
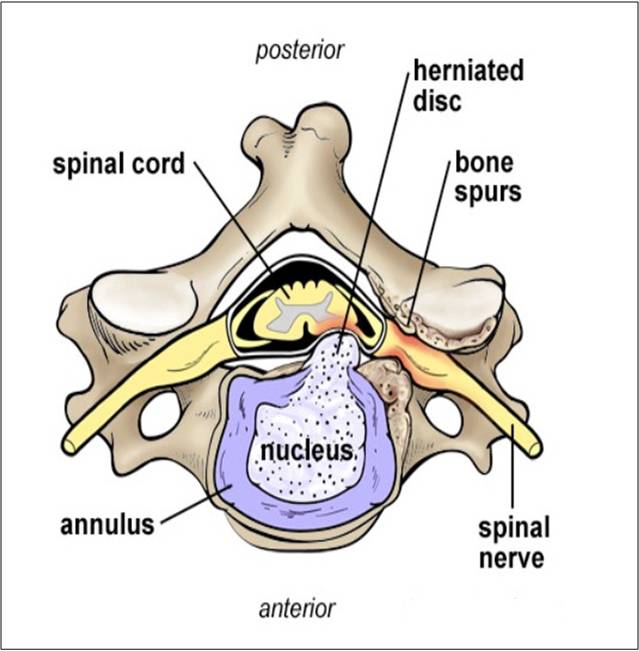
Fig. 1 Cervical Degenerative Disc Disease with leakage of jelly into the spinal canal and causing spinal cord compression or nerve root compression or inflammation of the nervous structure.
- Bulging and herniated disc: The gel-like material within the disc can bulge or rupture through a weak area in the surrounding wall (annulus). Irritation and swelling occurs when this material squeezes out and painfully presses on a nerve (Fig. 1).
- Degenerative disc disease: As discs naturally wear out, bone spurs form and the facet joints inflame. The discs dry out and shrink, losing their flexibility and cushioning properties. The disc spaces get smaller. These changes lead to foraminal or central stenosis or disc herniation.
Disc replacement has narrower indications. It is commonly not advisable if you have:
- Cervical instability
- Advanced disc degeneration with narrowed disc space
- Facet joint arthritis
- Osteoporosis
- Inflammatory arthritis
- Post traumatic condition with deformed anatomy
The surgical decision
Most herniated discs heal after a few months of nonsurgical treatment. Your doctor may recommend treatment options, but only you can decide whether surgery is right for you. Be sure to consider all the risks and benefits before making your decision. Only 20% of people with herniated disc problems have enough pain after 6 weeks of nonsurgical treatment to consider surgery [6].
Your surgeon will also discuss the risks and benefits of different types of bone graft material. Autograft is the gold standard for rapid healing and fusion, but the graft harvest can be painful and at times lead to complications. Autograft is more commonly used these days as it has proven to be as effective for routine one and two level fusions in non-smokers.
Who performs the procedure?
Ideally, spine surgeons who have specialised training in complex spine surgery should perform the surgery. Ask your surgeon about their training, especially if your case is complex or you’ve had more than one spinal surgery.


If you are having surgery with hong kong spine and pain centre, we will send you anaesthetic pre-assessment forms so that the surgeon and the anaesthetist know your medical history (allergies, medicines/vitamins, bleeding history, anaesthesia reactions, previous surgeries). You may be scheduled for presurgical tests (e.g., blood test, electrocardiogram, chest X-ray) the day before surgery.
Discuss all medications (prescription, over-the-counter, and herbal supplements) you are taking with your doctor. Some medications need to be continued or stopped some weeks before the surgery.
Stop taking all blood thinners 1 to 2 weeks before surgery as directed by the doctor. Stop taking non-steroidal anti-inflammatory medicines 2-3 days before the surgery is preferred. Additionally, stop smoking, chewing tobacco, and drinking alcohol 1 week before until 2 weeks after surgery because these activities can cause bleeding problems.
No food or drink is permitted past midnight the night before surgery.
Smoking
The most important thing you can do to ensure the success of your spinal surgery is quit smoking. This includes cigarettes, cigars, pipes, chewing tobacco, and smokeless tobacco (snuff, dip). Nicotine prevents bone growth and puts you at higher risk for a failed fusion. Patients who smoked had failed fusions in up to 40% of cases, compared to only 8% among non-smokers [7]. Smoking also decreases your blood circulation, resulting in slower wound healing and an increased risk of infection.


- Shower using antibacterial soap. Dress in freshly washed, loose-fitting clothing.
- If you have instructions to take regular medication the morning of surgery, do so with small sips of water.
- Remove make-up, hairpins, contacts, body piercings, nail polish, etc.
- Leave all valuables and jewellery at home (including wedding bands).
- Bring a list of medications (prescriptions, over the- counter, and herbal supplements) with dosages and the times of day usually taken.
- Bring a list of allergies to medication or foods.


There are seven steps to the procedure. The operation generally takes 2 to 3 hours.
Step 1: prepare
You will lie on your back on the operative table and be given anaesthesia. Once asleep, your neck area is cleansed and prepped. If a fusion is planned and your own bone will be used, the hip area is also prepped to obtain a bone graft. If a donor bone will be used, the hip incision is unnecessary.
Step 2: make an incision
A 2-inch skin incision is made on the right or left side of your neck (Fig. 2). The surgeon makes a tunnel to the spine by moving aside muscles in your neck and retracting the trachea, oesophagus, and arteries. Finally, the muscles that support the front of the spine are lifted and held aside so the surgeon can clearly see the bony vertebrae and discs.
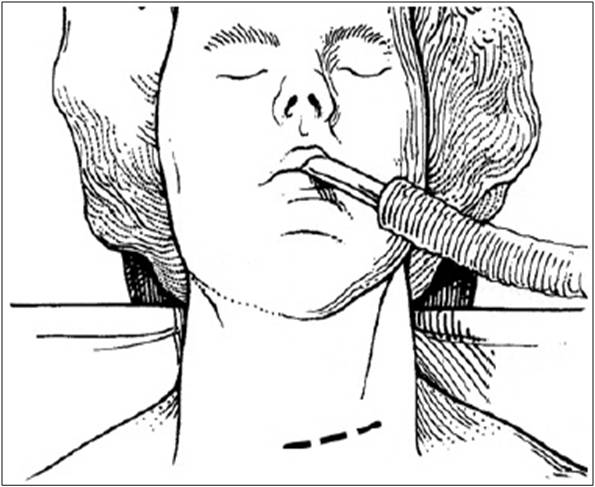
Fig. 2. Patient is in supine position under GA. A small cut at the front side of the neck. Left side approach as shown.
Step 3: prepare to remove disc
With the aid of a fluoroscope (a special video X-ray), the surgeon passes a thin needle into the disc to locate the affected vertebra and disc. To remove the damaged disc, the vertebrae above and below the disc must be held apart. Your surgeon first inserts a spreader into the body of each vertebra above and below the disc to be removed. Gentle tension is placed on the spreader to separate the two vertebrae.
Step 4: remove the disc fragments
The outer wall of the disc (annulus) is cut (Fig. 3). The surgeon removes about 2/3 of your disc using small grasping tools, and then looks through a surgical microscope to remove the rest of the disc. The posterior longitudinal ligament, which runs behind the vertebrae, is removed to reach the spinal canal. Any disc material pressing on the spinal nerves is removed.
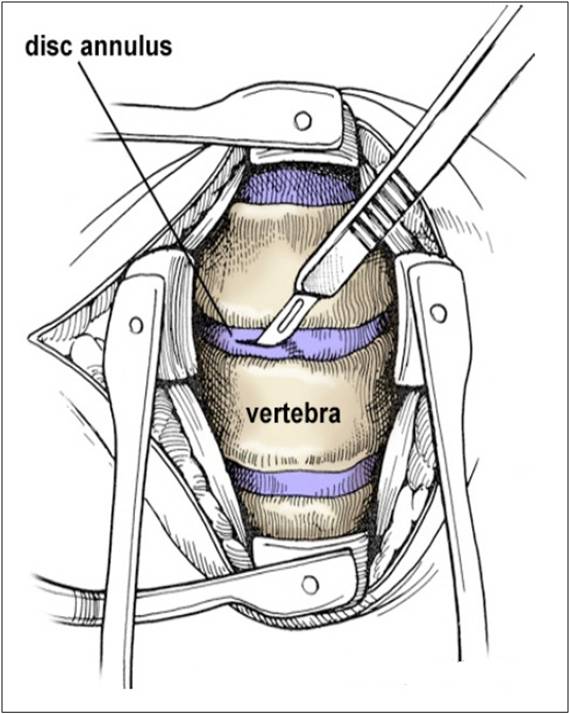
Fig. 3. After exposure of the cervical spine from the front, level of the disc will be confirmed by X-ray before making a cut on it. Decompression can be achieved when the dural sac seen from the front under microscope.
Step 5: decompress the nerve
Bone spurs (osteophytes) that press on your nerve root are removed. The foramen, through which the spinal nerve exits, is enlarged with a drill (Fig. 4). This procedure, called a foraminotomy, gives your nerves more room to exit the spinal canal.
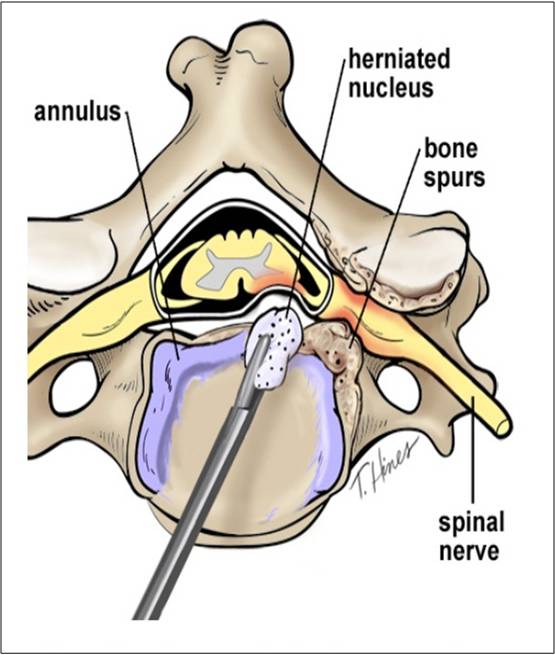
Fig. 4. Annulus and nucleus has been removed bit by bit under microscope. Bone spurs are removed with power blur.
Step 6. prepare a bone graft fusion
Using a drill, the open disc space is prepared on the top and bottom by removing the outer cortical layer of bone to expose the blood-rich cancellous bone inside. This “bed” will hold the bone graft material that you and your surgeon selected:
Conventional treatment: Cervical Spine Fusion with a Cage or Bone graft
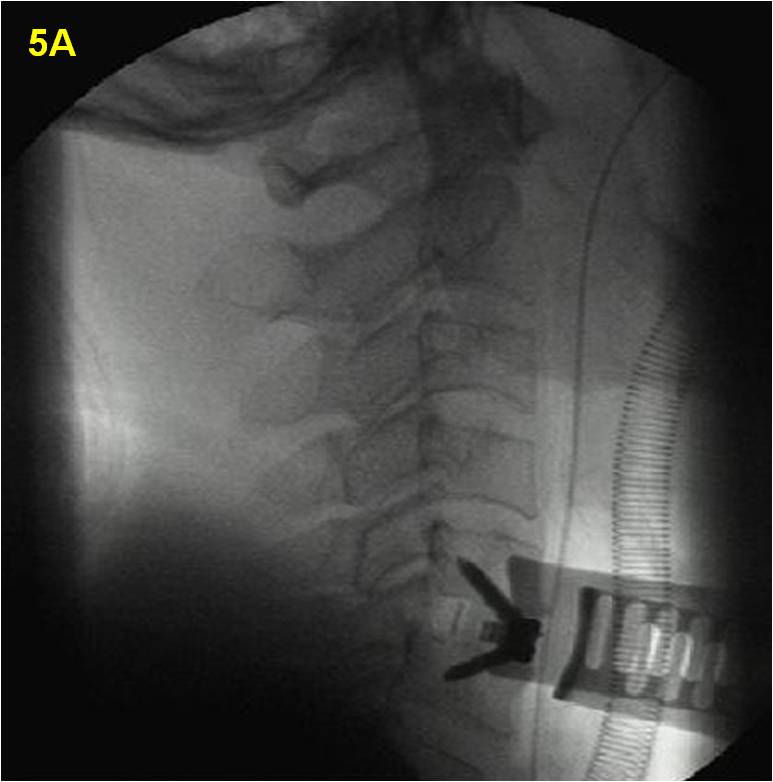
A bioplastic cage is filled with fully synthetic biologic bone substitute bone-growing agents (Fig. 5A). The implant is then tapped into the shelf space. Titanium screws are inserted into the vertebrae to provide stability during fusion – and possibly a better fusion rate. An x-ray is taken to verify the position of the bone graft and titanium fixation device (Fig. 5B).
|
|
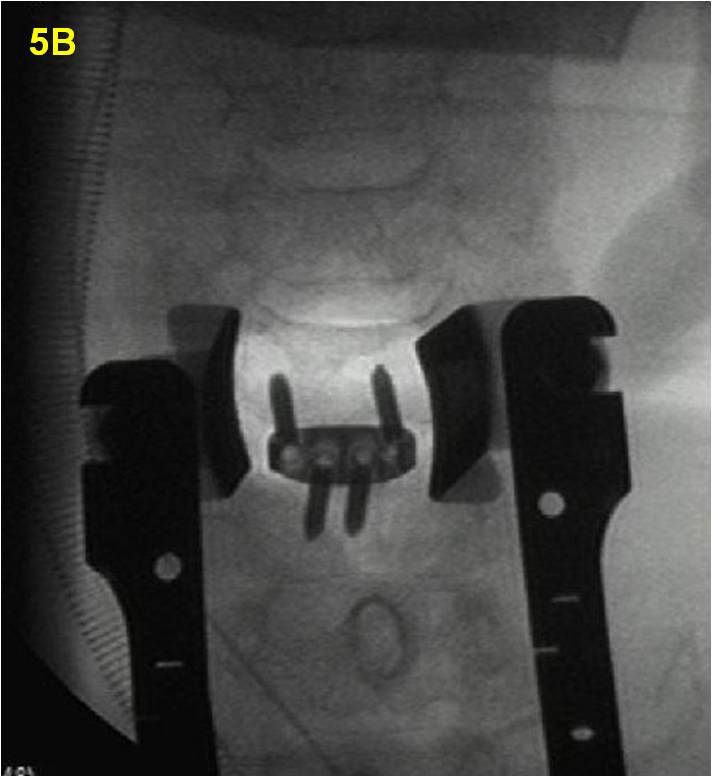 |
Fig. 5. Intra-operative X-ray screening during the ACDF procedure. The C56 cage and screw position is fully visualised to prevent spinal cord injury.
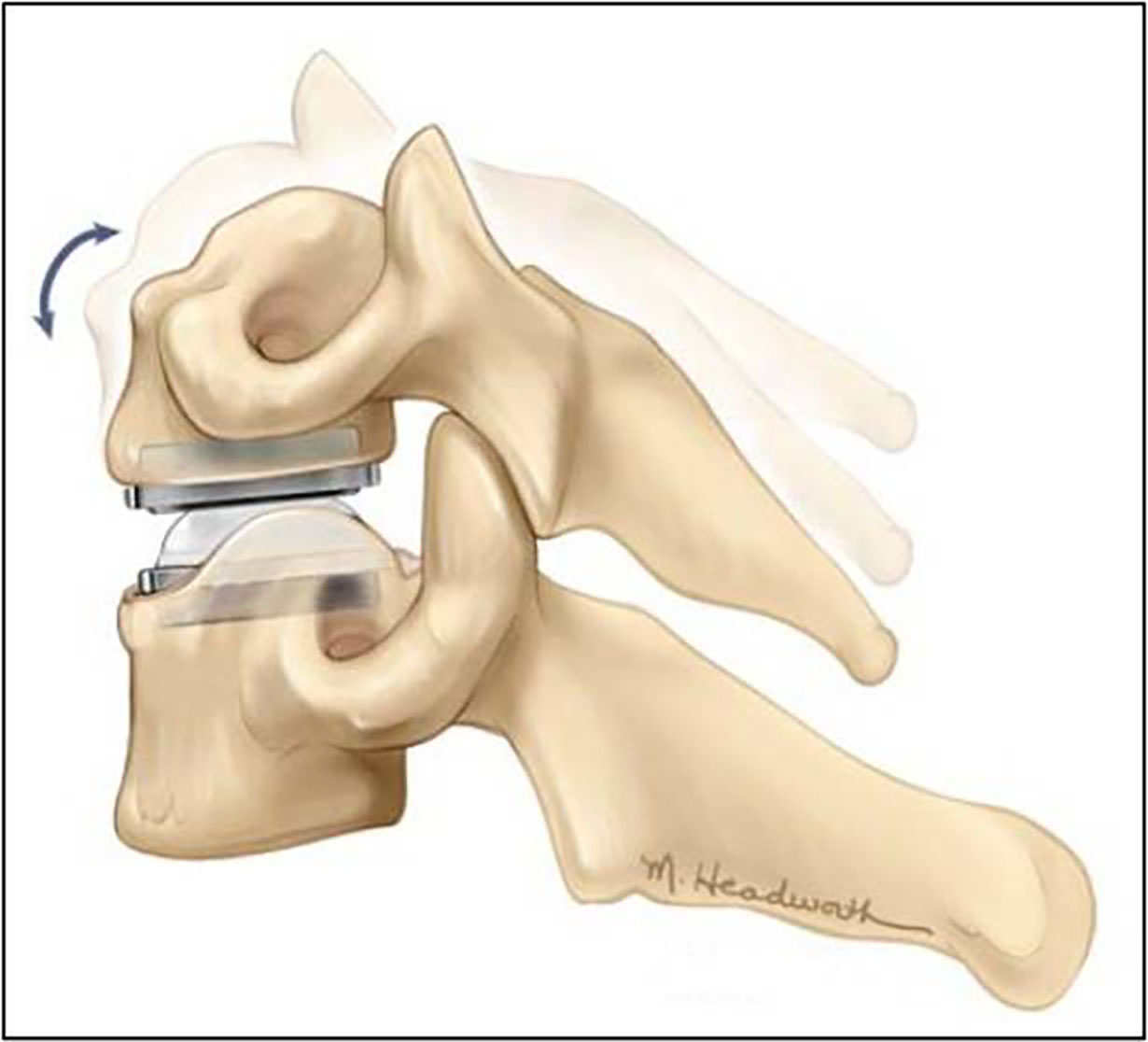
Alternative option: Artificial Disc Replacement
Instead of a bone graft or fusion cage, an artificial disc device is inserted into the empty disc space (Figs. 6 & 7). In select patients, it may be beneficial to preserve motion. Talk to your doctor – not all insurance companies will pay for this new technology and out-of-pocket expenses may be incurred.
|
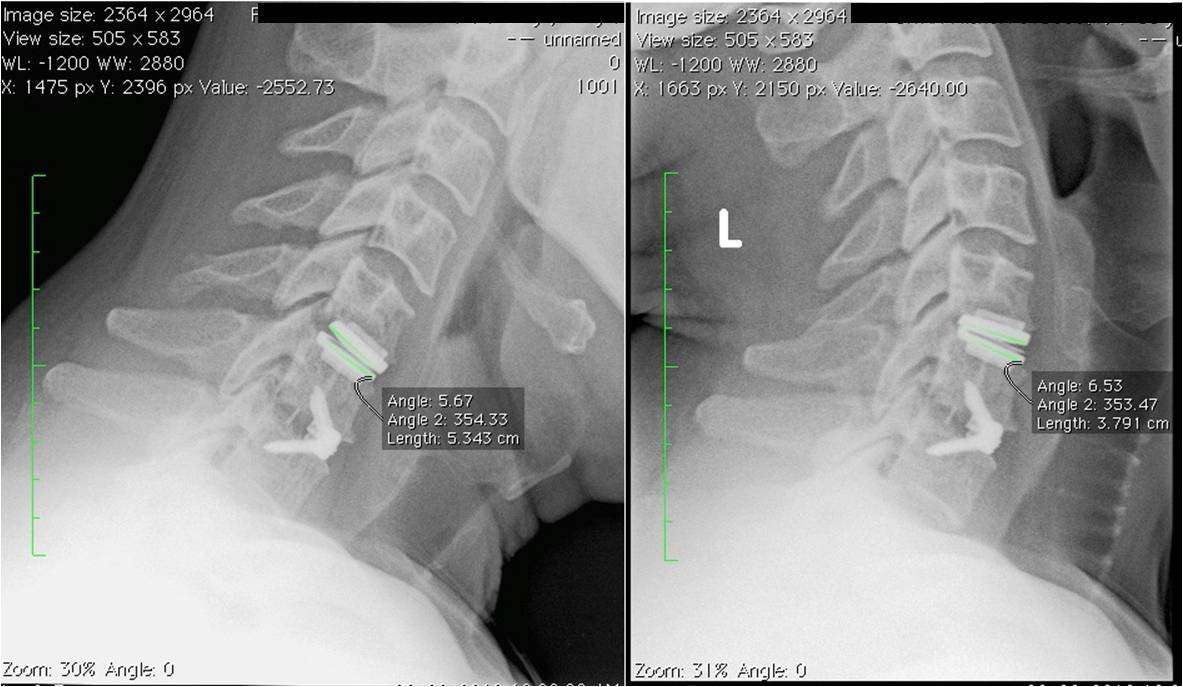
Fig. 6. Motion-preservative artificial disc replacement. There is 12-14 degrees of motion on flexion/extension. Lateral bending is around 10 degree. |
Fig. 7. Post op X-ray at 4 weeks after ACDF and ADR. The active range of motion can be up to 14 degrees in flexion extension views. |
Step 7. close the incision
The spreader and retractors are removed. The muscle and skin incisions are sewn together with sutures.
Steri-Strips is placed across the incision. A suction drain will be inserted during the surgery to act as a monitor of the internal bleeding and suck out the remaining blood stained fluid from the surgery site.


You will awaken in the postoperative recovery area. Blood pressure, heart rate, and respiration will be monitored. Any pain will be addressed. Once awake, you will be moved to a regular room where you’ll increase your activity level (sitting in a chair, walking). Most patients having a 1 or 2 level ACDF are sent home on the next day. However, if medical complications such as difficulty breathing or unstable blood pressure develop, you may need to stay for longer time in the hospital.


Discomfort
- After surgery, pain is managed with narcotic medication. Because narcotic pain pills are addictive, they are used for a limited period (2 to 4 weeks). As their regular use can cause constipation, drink lots of water and eat high fibre foods. Laxatives (e.g., Dulcolax, Senokot, Milk of Magnesia) can be bought without a prescription. Thereafter, pain is managed with acetaminophen.
- Hoarseness, sore throat, or difficulty swallowing may occur in some patients and should not be cause for alarm. These symptoms usually resolve in 1 to 4 weeks.
Restrictions
- If you had a fusion, short term use of non-steroidal anti-inflammatory drugs (NSAIDs) for 2-4 weeks is safe for the surgery.
Do not smoke. Smoking delays healing by increasing the risk of complications (e.g., infection) and inhibits the bones’ ability to fuse. - Do not drive for 2 to 4 weeks after surgery or until discussed with your surgeon.
Avoid sitting for long periods of time.
Avoid bending your head forward or backward vigorously. - Do not lift anything heavier than 5 pounds (e.g., gallon of milk).
- Housework and yard-work are not permitted until the first follow-up office visit. This includes gardening, mowing, vacuuming, ironing, and loading/unloading the dishwasher, washer, or dryer.
Activity
- You may need help with daily activities (e.g., dressing, bathing), but most patients are able to care for themselves right away.
- Gradually return to your normal activities. Walking is encouraged; start with a short distance and gradually increase to 1 to 2 miles daily. A physical therapy program may be recommended.
- If applicable, know how to wear a cervical collar before leaving the hospital. Wear it when walking or riding in a car.
Bathing/Incision Care
- You may shower the day after surgery when the suction drain has been taken off. Follow your surgeon’s specific instructions. No tub baths, hot tubs, or swimming pools until your health care provider says it’s safe to do so.
- There are no stitches requiring removal. There are only sterile strips on the skin to appose the incision. The strips can be removed at around 10 to 14 days after the surgery.
When to Call Your Doctor
- If your temperature exceeds 101° F, or if the incision begins to separate or show signs of infection, such as redness, swelling, pain, or drainage.
- If your swallowing problems interfere with your ability to breathe or drink water.
Recovery and prevention
Schedule a follow-up appointment with your surgeon for 2-4 weeks after surgery. Recovery time generally lasts 4 to 6 weeks. X-rays may be taken in the subsequent follow up visits. The surgeon will decide when to release you back to work or sports at your follow-up visit. A soft cervical collar is usually given to provide support and limit motion for 2 weeks. Your doctor will prescribe physical therapy once your neck wound has healed.
Residual neck pain are common after the surgery. The keys to minimising the pain are:
- Proper lifting techniques
- Good posture during sitting, standing, moving, and sleeping
- Appropriate exercise program
- An ergonomic work area
- Healthy weight and lean body mass
- A positive attitude and relaxation techniques (e.g., stress management)
- No smoking


What are the results?
Anterior cervical discectomy is successful in relieving arm pain in 92 to 100% of patients. However, arm weakness and numbness may persist for weeks to months. Neck pain is relieved in 73 to 83% of patients. In general, people with arm pain benefit more from fusion than those with neck pain. Aim to keep a positive attitude and diligently perform your physical therapy exercises. Achieving a spinal fusion varies depending on the technique used and your general health (and whether you smoke). In a study that compared three techniques: discectomy alone, without fusion, discectomy and fusion without plates and screws, and discectomy and fusion with plates and screws, the outcomes were [8]:
- 67% of people who underwent discectomy alone (no bone graft) achieved fusion naturally. However, discectomy alone results in an abnormal forward curving of the spine (kyphosis) compared with the other techniques.
- 93% of people who underwent discectomy and fusion with bone graft placement achieved fusion.
- 100% of people who underwent discectomy and fusion with bone graft placement and plates and screws achieved fusion.


What are the risks?
No surgery is without risks. General complications of any surgery include bleeding, infection, blood clots (deep vein thrombosis), and reactions to anaesthesia. The usually quoted complication rate is <1% [9].
Specific complications related to ACDF may include:
- Hoarseness and swallowing difficulties. In some cases, temporary hoarseness can occur. The recurrent laryngeal nerve, which innervates the vocal cords, is affected during surgery. It may take several months for this nerve to recover. In rare case (less than 1/250) hoarseness and swallowing problems may persist and need further treatment with an ear, nose and throat specialist [10].
- Vertebrae failing to fuse. Among many reasons why vertebrae fail to fuse, common ones include smoking, osteoporosis, obesity, and malnutrition. Smoking is by far the greatest factor that can prevent fusion. Nicotine is a toxin that inhibits bone-growing cells. If you continue to smoke after your spinal surgery, you could undermine the fusion process.
- Hardware fracture. Metal screws, rods, and plates used to stabilise the spine are called “hardware.” The hardware may move or break before your vertebrae are completely fused. If this occurs, a second surgery may be needed to fix or replace the hardware. This is rare.
- Bone graft migration. In rare cases (1 to 2%), the bone graft can move from the correct position between the vertebrae soon after surgery. This is more likely to occur if hardware (plates and screws) are not used to secure the bone graft. It’s also more likely to occur if multiple vertebral levels are fused. If this occurs, a second surgery may be necessary [11].
- Adjacent-segment disease. This syndrome occurs when the vertebrae above or below a fusion take on extra stress. The added stress can eventually degenerate the adjacent vertebrae and cause pain [12]. Cervical Disc Replacement (ADR) is a newer technology for treating cervical disc degeneration or hernia. The artificial disc performs like an artificial joint to serve some motion on flexion extension of the neck. It has potential advantages to prevent the stress migrating to the level above the index level. The increase of intra-discal pressure might accelerate the disc degeneration. However, it is only indicated for early cervical disc degeneration with well preserved anatomy. Cervical facet joint arthritis, osteoporosis, inflammatory arthritis, abnormal cervical spinal anatomy, osteoporosis (soft bone) are not suitable for this surgery. For single level cervical disc degeneration/hernia, anterior cervical discectomy and fusion is still the gold standard of treatment. The functional loss is negligible for single level fusion [13].
- Nerve damage or persistent pain. Any operation on the spine comes with the risk of damaging the nerves or spinal cord. Damage can cause numbness or even paralysis. Sometimes, your surgeon may recommend intra-operative neuromonitoring to monitor the effect of the decompression and also prevent neurological insult during the surgery. However, the most common cause of persistent pain is nerve damage from the disc herniation itself. Some disc herniations may permanently damage a nerve making it unresponsive to decompressive surgery. Be sure to go into surgery with realistic expectations about your pain. Discuss your expectations with your doctor.


Cervical disc hernia with spinal cord or nerve root compression is a common disease. It is common younger population including those without special risk factors. Surgical treatment has good outcomes if conservative treatment fail. The surgical risk is not high. There are newer technology to overcome the problem of the past in reducing the surgical risk and speeding recovery.


- Robinson RA, Smith G (1955) Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp 96:223–224; Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15:602–617.
- Kulkarni AG, Hee HT, Wong HK (2007) Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J 7(2):205–209.
- Comparison of 3 Fusion Techniques in the Treatment of the Degenerative Cervical Spine Disease. Is Stand-Alone Autograft Really the “Gold Standard”: Prospective Study With 2-Year Follow-up Vanek P, Bradac O, Delacy P, Saur K, Belsan T, Benes V. Spine (Phila Pa 1976). 2012 Sep 1;37(19):1645-51.
- J Spinal Disord Tech. 2010 Feb;23(1):15-21. Normal functional range of motion of the cervical spine during 15 activities of daily living. Bible JE, Biswas D, Miller CP, Whang PG, Grauer JN.
- Nabhan A, Ahlhelm F, Shariat K, Pitzen T, Steimer O, Steudel WI, Pape D (2007) The ProDisc-C prosthesis: clinical and radiological experience 1 year after surgery. Spine 32(18): 1935–1941.
- Einstadter D, Kent DL, Fihn SD, Deyo RA. Med Care. 1993 Aug;31(8):711-8. Variation in the rate of cervical spine surgery in Washington State.
- Hilibrand AS, et al.: Impact of smoking on the outcome of anterior cervical arthrodesis with interbody or strut-grafting. J Bone Joint Surg Am 83- A:668-73, 2001.
- Xie JC, Hurlbert RJ. Discectomy versus discectomy with fusion versus discectomy with fusion and instrumentation: a prospective randomized study. Neurosurgery 61:107-16, 2007.
- Spine (Phila Pa 1976). 2007 Oct 1;32(21):2310-7. Anterior cervical discectomy and fusion associated complications. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, Lee GP, Robinson JS Jr.
- Spine (Phila Pa 1976). 2010 Apr 20;35(9 Suppl):S76-85. Postoperative dysphagia in anterior cervical spine surgery. Riley LH 3rd, Vaccaro AR, Dettori JR, Hashimoto R.
- J Clin Neurosci. 2009 Mar;16(3):373-7. Epub 2009 Jan 12. Acute graft extrusion following central corpectomy in patients with cervical spondylotic myelopathy and ossified posterior longitudinal ligament. Kumar GS,Rajshekhar V.
- Wigfield C, Skrzypiec D, Jackowski A, Adams MA (2003) Internal stress distribution in cervical intervertebral discs: the influence of an artificial cervical joint and simulated anterior interbody fusion. J Spinal Disord Tech 16:441–449.
- Orthop Surg. 2012 May;4(2):94-100. doi: 10.1111/j.1757-7861.2012.00176.x. Motion analysis of single-level cervical total disc arthroplasty: a meta-analysis. Chen J, Fan SW, Wang XW, Yuan W.
All Rights Reserved. Web Design by YSD