Anatomy of the spine
The spine needs to be both strong and flexible, and therefore consists of strong bones – the vertebrae – separated by flexible soft tissues – the intervertebral discs and facet joints (Fig. 1).
The bodies of the vertebrae are at the front, the facet joints, laminae and spinous processes are at the back, and the spinal cord and the nerves are protected in between them.
The intervertebral discs are between the vertebral bodies and act as shock absorbers. They have a tough outer ring called the annulus fibrosus and a jelly-like centre called the nucleus pulposus (Fig. 2A).
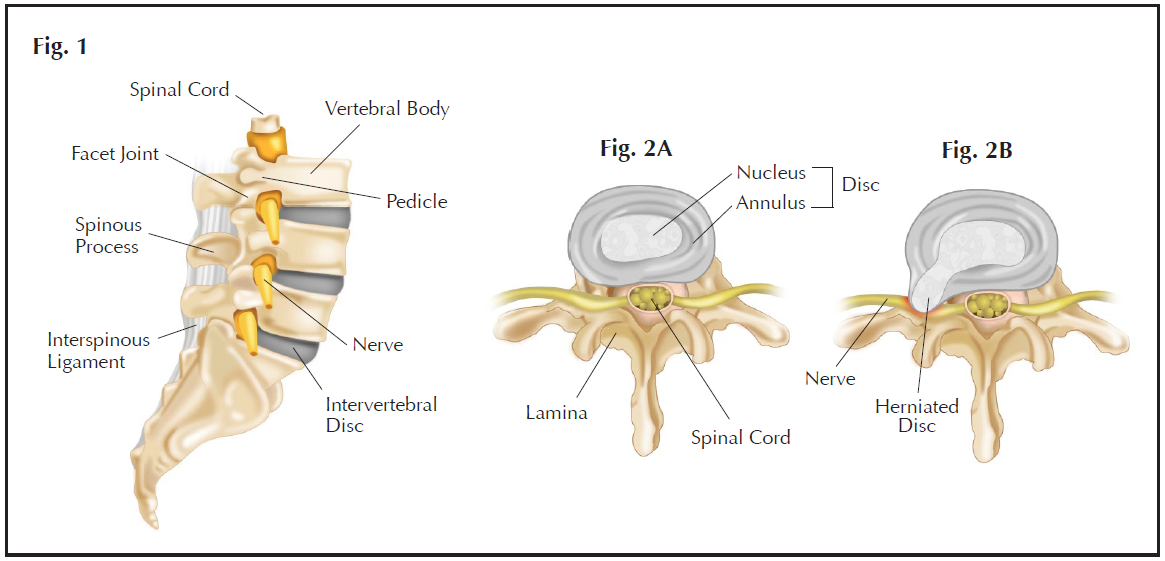
Fig. 1 Anatomy of the spine showing: the lumbar vertebrae; intervertebral discs; spinal cord and nerves; pedicles; facet joints; spinous processes and interspinous ligaments. The laminae are not visible in this side view.
Fig. 2A Normal intervertebral disc.
Fig. 2B A “slipped disc” – the annulus fibrosus has torn and the nucleus pulposus has herniated through the tear, compressing a lumbar spinal nerve, which could cause pain in the nerve’s territory - the symptom of sciatica.
<
What is a ‘slipped disc’?
‘Slipped disc’ is a colloquial term for a burst (or prolapse or herniation) of the intervertebral disc. This is much like a jam doughnut bursting and the jam coming out. From early adulthood, the annulus fibrosus becomes weaker[1]. As a result, the intervertebral disc is more vulnerable to the pressure of the body’s weight. If the annulus fibrosus tears, the jelly like nucleus pulposus leaks out to become a herniated disc (Fig. 2B).
If a herniated disc compresses on the nerves, it may cause pain, tingling, numbness or weakness of the leg, symptoms known as sciatica. Patients may also experience back pain with a herniated disc, although back pain can have many causes other than a herniated disc.


What are the symptoms of a slipped disc?
The symptoms depend on where the disc has herniated, and what spinal nerve root it is compressing or irritating. Different patients may have different symptoms.
The most common symptoms of slipped disc include:
- Low back pain. This may be continuous or intermittent. It can be also worsened by coughing, sneezing, prolonged standing, or particular movements.
- Buttock pain and hip pain.
- Back muscle spasm.
- Sciatica. When a herniated disc is pushing on certain nerves, patients may find the pain that starts from the buttock or back of the thigh and travels down the leg to the calf, sole of the foot, or even to the toes. This usually affects only one leg, but occasionally it can affect both legs. (Fig. 3)
- Numbness or tingling in the leg or foot.
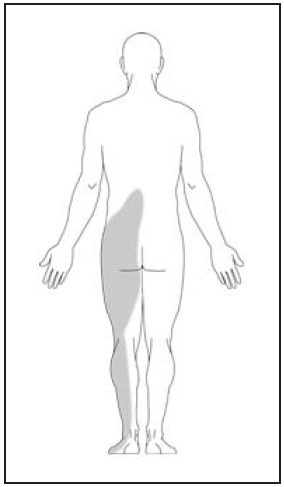
Fig. 3 Typical location of pain in sciatica: Shooting pain and numbness starts from the buttock, then travels down to back of the thigh and the leg, even to the foot.
Some patients experience alarming symptoms:
- Weakness of the leg, foot, or toes. This may appear as a limp, with a typical ‘foot drop’ or it may be too subtle to be noticed by the patient, but a careful physical examination by an experienced doctor can reveal the problem.
- Loss of bowel or bladder function. Nerves to the bladder or bowel may be affected, resulting in partial or complete loss of urinary or faecal sensation or control. This is an emergency. If you experience these problems, seek medical attention immediately – you will most likely require an emergency operation.


What are the risk factors for slipped disc?
You have higher chance of lumbar disc herniation if you have the following risk factors [2, 3]:
- 30 - 50 years of age
- Smoking
- Overweight
- Male
- History of back pain
- Lack of exercise
- Occupation or specific activities which require:
- prolonged sitting and standing
- bending forward or backward
- frequent heavy lifting
- vibration to the back, e.g. driving
- frequent night shifts


How is a slipped disc diagnosed?
Your doctor will carefully listen to your story and examine you, and usually he will arrange MRI scan.
Magnetic Resonance Imaging (MRI). MRI is extremely useful for assessing the spine as it shows the spinal cord, nerve roots and other soft tissues as well as the bones. MRI produces cross-sectional images in three planes, allowing doctors to get a clear understanding of the anatomy. The special weight bearing MRI scanner which takes images with the individual standing up – this can be helpful, as lumbar disc herniations are sometimes only present when one is standing [4-6] (Figs. 4 & 5).


Fig. 5A MRI showing a herniated disc protruding into spinal canal at L5/S1 level (arrow).
This is a longitudinal plane image – as if looking at the spine from the side.
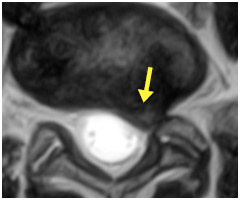
Fig. 5B Horizontal plane image of the same MRI at L5/S1 level showing
the disc herniation pressing on the left S1 nerve (arrow).
Are any other tests required?
MRI is most useful, but sometimes other tests can be helpful as well.
X-rays
X-rays can show the bones, but not the soft tissues. They are useful in ruling out some other causes of low back pain, for instance, fractures, spinal instability and tumours. However, in most cases of acute lumbar disc herniation, X-rays of the lumbar spine do not show any abnormality, or show non-specific changes.
Computed Tomography (CT) scan
CT scanning shows the bone in high resolution in three dimensions, but it does not show soft tissue as well as MRI.
Electromyogram and Nerve Conduction Test
The electromyogram (EMG) measures the electrical activity of muscle at rest and during contraction, while the nerve conduction test measures how well and how fast the nerves carries electrical signals. These tests can quantify the severity with which the nerve and its related muscle group have been affected due to nerve compression. They can also help to locate the site of nerve compression particularly if the diagnosis is not clear.


What is the treatment?
Lumbar disc herniation usually recovers on its own, and, therefore, one should try non-operative treatment first. Operation is recommended if the symptoms have not improved or are getting worse after about 6 to 8 weeks of non-operative treatment, because operative results seem to get worse after 60 days of symptoms [7].
Rest
This is the best and easiest way to relieve pain in the acute phase of lumbar disc herniation.
- take a few days off work.
- lie on a medium-firm bed on your side with a pillow between your knees (in order to relax your back and core muscles and to avoid spasm). The pressure on the lumbar spine and intervertebral discs is relieved.
- after a few days, if you are well enough, you should start walking short distances and doing light exercises.
Medicine
Oral pain medications usually work best if you take them early and on a regular schedule, instead of waiting until the pain is severe. Non-steroidal anti-inflammatory drugs (NSAIDs) are the first choice to reduce inflammation and pain. Modern COX-2 selective NSAIDs have all the advantages but fewer side-effects of the conventional NSAIDs. Some drugs have been developed particularly for nerve pain, they might have extra advantages in reducing the radiating leg pain in slipped disc. One common side effect is drowsiness – which can be quite helpful.
Physiotherapy
Physiotherapists will tailor-make a physical programme according to your symptoms and disabilities [8], initially to improve pain and then to improve the strength, flexibility, and endurance of the back and core muscles.
Epidural Steroid Injection
When a slipped disc is compressing a nerve, patients may feel pain because the nerve is irritated and inflamed. Epidural steroid injection is a minimally invasive procedure to reduce the inflammation and thus to relieve the pain and discomfort.
There are two ways of performing an epidural steroid injection: interlaminar and transforaminal. Transforaminal injection limits the injection to a smaller area and is more targeted, and is therefore our preferred technique.
How is transforaminal epidural steroid injection performed?
A spinal nerve exits the spinal canal through a side-hole called the neural foramen. This is also one of the commonest sites where spinal nerves are compressed by slipped discs. The procedure of transforaminal epidural steroid injection (TESI) is performed by a spine surgeon or pain specialist in an operating room or a special procedure suite, because video X-ray is required. A thin needle is inserted just above the nerve root near the neural foramen under X-ray guidance. A mixture of a long-lasting corticosteroid and a local anaesthetic is injected around the nerve root in order to reduce the inflammation and pain (Fig. 6).
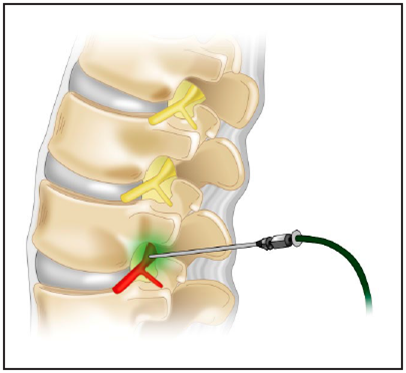
Fig. 6 A thin needle is carefully positioned to inject steroid medications around the inflamed nerve during TESI.
What are the results?
Patient can go home the same day. Many people feel a little better immediately, but it takes one to two weeks for the full benefit of the treatment to be felt. Most patients feel better after TESI [9, 10]. As the pain is reduced, physiotherapy will switch from pain relief to regaining strength and motion. Although TESI reduces swelling associated with disc herniation, it cannot reduce the size of the disc herniation itself.
Who benefits most from TESI?
Patients who have small to medium sized slipped discs, but suffer from significant radiating leg pain and numbness, and do not respond to rest and medicine, benefit most because their symptoms are usually caused by nerve irritation and inflammation.
TESI should not be performed on patients who: are pregnant; have an infection; have bleeding problems; or have uncontrolled diabetes.
What are the risks?
TESI is a minimally invasive procedure. It is relatively safe and has only few risks. Patient might experience a temporary increase in leg numbness or weakness from the local anaesthetic blocking the nerves. This usually resolves within 8 - 12 hours as the anaesthetic wears off. The procedure also carries a small risk of headache (due to dural puncture, allowing some of the cerebrospinal fluid, in which the brain floats, to escape); infection (very rare), bleeding (rare), nerve damage (rare), allergic reaction (rare), corticosteroid side-effects (very rare), or paralysis (extremely rare) [11, 12].
What about operation?
Although most of lumbar disc herniation can be treated non-operatively, studies show that operation can achieve a faster relief in leg symptoms [13] and better long-term outcome and satisfaction compared with nonoperative treatment [14,15].
Operation is recommended if there is:
- Cauda Equina Syndrome (loss of bladder or bowel sensation or control).
- Significant muscle weakness.
- No response to non-operative treatment after 6-8 weeks.
- Significant functional disability due to severity of symptoms.
- Very large disc or disc fragments which have come away from the rest of the disc (know as a ‘sequestrated’ disc).
What does operation involve?
The most usual operation is ‘discectomy’. This is the surgical procedure to remove the herniated parts of the intervertebral disc. It does not remove the entire disc. The operation is performed in hospital with the aid of an anaesthetic.
In the conventional technique of discectomy, an incision is made in the skin and the back muscles are moved to the side so that the surgeon can see the laminae (the bone forming the back of the vertebra).
A bone opening (called a ‘laminotomy’) is created between two laminae to allow the surgeon to see the spinal canal. The nerve root is moved out of the way, the herniated intervertebral disc is exposed and the surgeon removes the loose disc material to relieve the pressure on the nerve (Fig. 7).
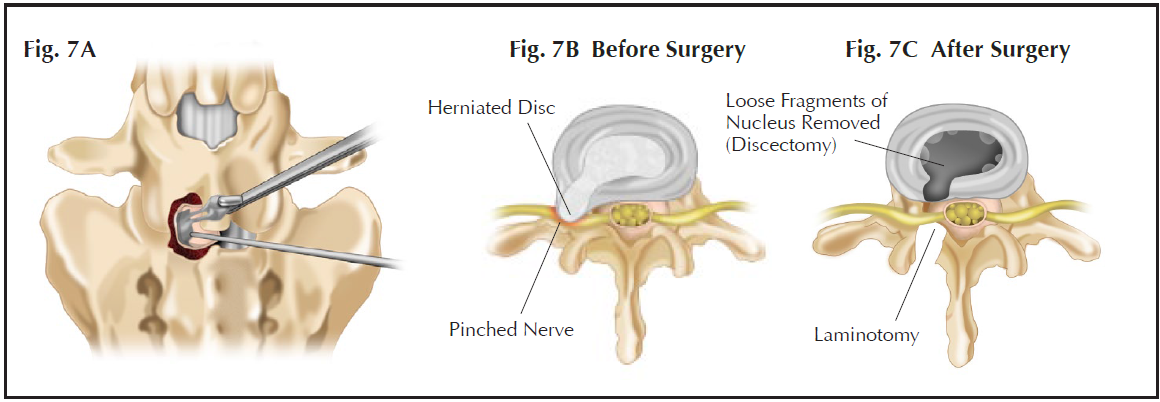
Fig. 7A A schematic diagram showing how the “slipped disc” can be removed during discectomy.
Fig. 7B A herniated disc is compressing on a spinal nerve causing sciatica before surgery.
Fig. 7C The spinal nerve is no longer compressed after discectomy.
Two recent refinements, microdiscectomy and endoscopic discectomy, produce better results and quicker recovery by allowing the surgeon a magnified view through a smaller incision.
Mircrodiscectomy
Using an operating microscope and special instruments the surgeon performs a similar procedure to a conventional discectomy via a smaller incision.
Endoscopic Discectomy
The recent development of endoscopic surgery of spine allows surgeon to perform discectomy with an even smaller skin incision. A tiny camera is inserted into the spinal canal through a very small hole (Fig. 8). The surgeon looks at the monitor screen.
The main advantage of microdiscectomy and endoscopic discectomy over the conventional approach is that the smaller incisions cause less damage to normal tissue and, because of the magnification, the surgeon can see better. Therefore, patients may recover faster and return to normal activity earlier.
 |
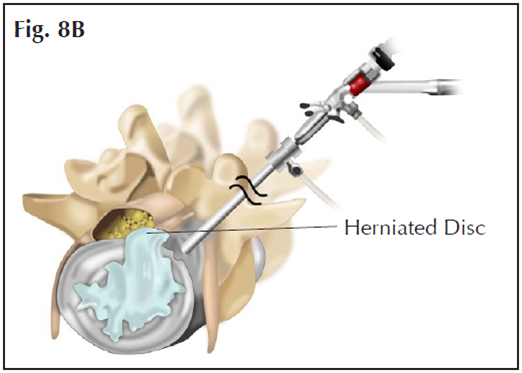 |
Figs. 8A&B An endoscopic discectomy using an endoscope and special instruments is performed through a very small skin incision.
How will I be after the operation?
After the operation, you will wake up in your hospital bed. You will have a drip providing fluid for a few hours, until you are ready to drink normally. You will not have any other tubes or drains. You will be able to get up and walk as soon as you feel well enough – usually after a few hours, certainly by the next day. The physiotherapists will make sure you can walk, climb stairs, and go to the bathroom safely and independently.
Usually you will stay in hospital for one night and you may go home as soon as you are safe and independent. You may be given a lumbar corset for comfort. Mild pain medicine will be given to you in hospital and you will normally continue on the same medicine for as long as needed – usually about 2 weeks. Normally you will attend out-patient physiotherapy. You will have waterproof ‘Gore-tex type’ dressings over your incision, and you will be able to shower normally. Usually the dressings will not require changing. You will see your surgeon in the office about 2 – 3 weeks after the operation. The dressings will be removed. The stitches dissolve, and do not need to be removed.
It is safe to walk as much as is comfortable, but avoid twisting, bending, or lifting objects over 5 lbs (2kgs).
You can travel by air as soon as you are discharged from the hospital. You should not lift heavy luggage - ask for help putting any luggage into the overhead compartment.
You should not drive until you have seen your surgeon at follow up, and he has confirmed that it is safe.
If your work is light, you may return to work as soon as you are comfortable, usually within two weeks. If your work is heavier, you can return to work when your back is strong enough.
What are the results of discectomy operation?
A lumbar discectomy is about 85% - 90% successful in relieving pain in the buttocks and legs. The results are similar regardless of the different methods of lumbar discectomy [15-17]. Some reports suggest that early surgery results in better pain relief and faster recovery than prolonged non-operative treatment [18]. Usually the pain and numbness of the leg is much relieved immediately after the surgery, although in some cases
it may takes several weeks for the symptoms to improve. However, if a nerve has been compressed for a long time, there are often permanent residual symptoms, typic ally mild numbness, pain, or weakness.
Most people recover quickly after a lumbar discectomy operation, and have no further problems, but lumbar discectomy is not a solution to the problem of disc degeneration. The main purpose of the operation is to remove pressure on the nerves, it is not intended to reverse the aging process of the disc.
Two problems are most common after lumbar discectomy: remaining nucleus pulposus may herniate again causing a “recurrent slipped disc” (5 - 15% incidence); or the unstable disc may be painful, typically causing episodic low back pain (10 – 25% incidence). The risk of these problems is affected by many factors, including smoking, obesity, the affected disc level, the type of herniation, the amount of disc removed [19-21].
If there is a ‘recurrent slipped disc’, revision surgery of lumbar discectomy is helpful if non-operative treatment is not successful.
If there is continued back pain after discectomy, lumbar fusion or lumbar disc replacement may be necessary, and usually solves the problem.
What are the risks?
Although a lumbar discectomy is a major surgery that requires anaesthesia, the chances of complications are low (total 2 - 8%) [16, 22, 23].
Important complications include:
Nerve injury (0.3%). This is the complication about which people worry the most, but it is fortunately rare. Patients may develop new muscle weakness after surgery. The nerve damage may be permanent. The chance of paraplegia (total weakness of both lo wer limbs) after surgery is extremely low.
Dural tear (4%). The dural sac is the fibrous membrane that contains the cerebrospinal fluid in which the spinal cord and spinal nerves float. Tears of the dural sac are usually small, and can usually be sealed quite simply. They usually have no major consequences, but patients may need to stay in bed for 4-5 days in order to prevent cerebrospinal fluid leakage.
Incisional haematoma (2%). This is a bruise in the wound, which may be uncomfortable, but usually has no major consequences.
Infection (5%). It is quite common to have a superficial wound infection. It is usually self-limiting and can be successfully treated with oral antibiotics. Deep wound infection is more serious, usually requiring intravenous antibiotics, and sometimes further surgery, but fortunately it is r are (0.3%).
Can I prevent slipped discs?
Maintain a healthy body weight. This helps reduce the burden on the lumbar spine and avoids overload stresses on intervertebral discs.
Don’t smoke. Smoking probably causes disc damage b y reducing the blood supply to the tissues.
Exercise regularly to maintain the strength and flexibility of the back and core muscles to support the lumbar spine. Pilates type exer cises are best.
Maintain correct sitting and standing posture. Use proper techniques and posture when lifting. For heavy loads, get help or use appropriate aids.


- Lumbar disc herniation is a common problem causing back pain and sciatica in young adults.
- It usually recovers on its own.
- Non-surgical treatment consists of rest, painkillers, physiotherapy, steroid injection.
- Occasionally people may have severe symptoms such as severe muscle weakness or loss of bladder or bowel sensation or control (cauda equina syndrome). This is an emergency, and patients should seek medical attention immediately.
- Transforaminal Epidural Steroid Injection (TESI) is a minimally invasive procedure which usually reduces symptoms significantly.
- If symptoms continue after 6 – 8 weeks, it is appropriate to have lumbar discectomy operation.
- Surgical treatments for lumbar disc herniation can achieve a faster relief in leg symptoms and better long-term outcomes and satisfaction compared with nonsurgical treatment.
- Modern surgical techniques using a microscope or video endoscope allow a good view through a very small incision, giving quick recovery and a low complication rate.
- Sometimes the disc material can prolapse again, giving a ‘recurrent slipped disc’. This is usually treated by repeat operation.
- 10 – 25% of people with slipped discs will develop back pain, which will require alternative treatment.
All Rights Reserved. Web Design by YSD


